A 42-year-old man, who is a father, husband, and son, arrives at the emergency room suffering from an intense headache that has worsened over the past months. Today, it is unbearable. He has no notable medical history to account for the headaches and is not on any regular medication. However, he is a smoker, and his blood pressure is alarmingly high at 210/100 mmHg (normal is below 120/80 mmHg). After conducting a range of tests, including blood and urine analyses, doctors diagnose him with significant kidney damage—stage four chronic kidney disease. If he progresses to stage five, he will require dialysis or a kidney transplant, making the situation quite severe.
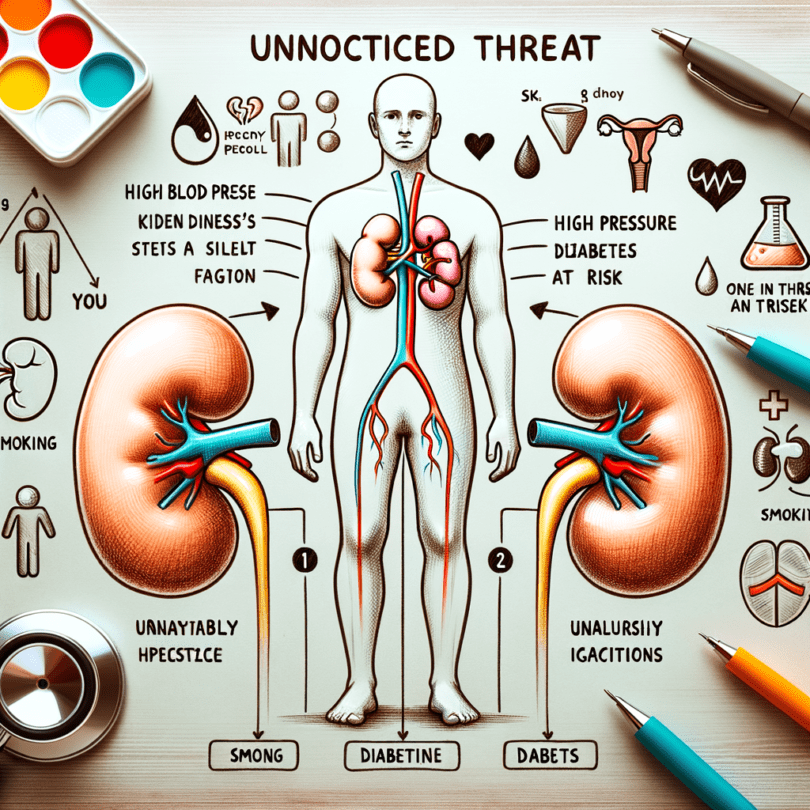
Kidney disease is often silent, with one in ten Australian adults showing signs of chronic kidney disease, many without realizing it. It is common for symptoms to emerge only after losing 90% of kidney function. Symptoms such as nausea, appetite loss, lethargy, and difficulty concentrating are common in kidney failure, but they are rather unspecific. Fluid retention, indicated by swollen ankles and puffy eyes, can signal kidney disease because the kidneys are crucial for regulating body fluid, and damaged kidneys cannot perform this function efficiently. Doctors use blood and urine tests to confirm kidney disease. Blood tests indicate kidney function percentage, while urine tests for blood and protein highlight signs of damage and inflammation. As kidneys eliminate waste and excess fluid from the body, their declining function leads to fluid and toxin build-up, causing swelling and difficulty breathing, and contributing to symptoms like fatigue and nausea.
High blood pressure may result from the diminished kidney function and can, in turn, worsen kidney condition by damaging their delicate filters, causing scarring. Individuals with chronic kidney disease have a 20-fold higher risk of dying from a heart attack or stroke. Consequently, heart complications often precede reaching end-stage kidney disease, where kidneys fail to meet the body’s required functions.
Healthy kidneys produce erythropoietin or EPO, a hormone stimulating red blood cell production. Declining kidney function reduces EPO production, leading to anemia, so patients require EPO injections to maintain red blood cell levels. Kidneys also help balance calcium and phosphate in the blood, with imbalances causing severe itching and potential bone fragility.
Kidney disease results from various factors, with one in three Australians having at least one risk factor for the disease. Indigenous Australians, especially those in remote areas, are at significant risk. Family history increases vulnerability, and additional risks include diabetes, high blood pressure, smoking, obesity, high cholesterol, heart disease, stroke, and age over 60. The prevalence of chronic kidney disease is projected to rise by 60% by 2020 due largely to the increasing rates of diabetes and obesity.
Individuals who have experienced acute kidney injuries may later develop chronic kidney disease. Inflammation of the kidneys or glomerulonephritis is a less common cause, often triggered by infections. While causes of many forms of glomerulonephritis are unknown, it can arise from infections like streptococcal, particularly in Indigenous Australian children in remote areas, where 15-20% are affected. Autoimmune responses or infections like hepatitis B or C can also trigger it.
Long-term use of certain medications can exacerbate kidney function decline. For instance, Bex, a painkiller popular in the 1960s caused severe kidney damage, leading to its discontinuation. Currently, anti-inflammatory drugs pose risks by limiting kidney blood flow, potentially resulting in acute kidney failure.
Other causes include cysts in the kidneys (polycystic kidney disease), congenital abnormalities, and damage from urine backflow into the kidneys (reflux nephropathy). Chronic kidney disease is incurable and hard to stop once it begins, highlighting the importance of early detection and lifestyle changes like weight loss, quitting smoking, managing blood sugar levels, and healthy eating to help control blood pressure and slow disease progression. Reducing dietary protein can also slow progression, though adherence is challenging.
Patients with chronic kidney disease require ongoing monitoring to manage declining function and prevent complications such as anemia, bone disease, malnutrition, and heart disease. The risk of progression to end-stage kidney disease is significant, necessitating dialysis or a transplant, costing Australia approximately A$1 billion annually, with demand for these treatments expected to rise by 60% by 2020.
Dialysis is necessary when toxins cannot be removed from the blood due to advanced kidney disease, requiring a machine to clean the blood of excess fluid and waste. Although it is a lifesaving measure, it greatly impacts quality of life. The life expectancy of those on dialysis is notably reduced compared to the general population, with only 46% surviving for five years, which is worse compared to many cancers.
When kidneys deteriorate to the point of needing replacement, a transplant offers a better quality and longer life, yet life expectancy post-transplant still trails a typical age-matched population. Those who have undergone transplants face heightened risks of heart disease and cancer. Demand for kidney transplants is rising, but donor organ availability hasn’t kept pace. In 2015, of 949 transplants conducted, there were still over 1,000 people waiting. The median wait time for a transplant was 2.4 years, and it is expected to increase given the rising demand.